A College of Charleston professor has developed a new technique for analyzing brain scans that could lead to a major breakthrough in how and when children are diagnosed with autism.
Computer science professor Brent Munsell has created a new computational model aimed at detecting abnormal brain growth in infants that correlates to a higher risk for developing autism. For the first time the technology offers doctors a tangible way to diagnose the neurodevelopmental disorder in infancy, rather than relying solely on behavioral cues as a child grows.
“Typically an autism diagnosis is made when a child is 24 months of age, and by that time it’s too late,” says Munsell. “With this new model, we can predict if a child is likely to have autism before age two and if it looks like he or she is at high risk, they can start treatments and therapies sooner.”
The cutting-edge technology is part of the Infant Brain Imaging Study (IBIS), a consortium of eight universities across the United States and Canada researching early brain development and autism.
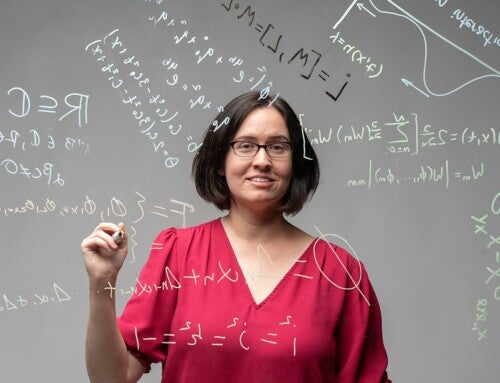
Munsell, in collaboration with professors at the University of North Carolina and New York University, created the new computational model at the College’s Machine Learning and Medical Image Analysis Lab. The project is one of several research initiatives Munsell oversees at the high-tech computer lab, many of which focus on new technologies aimed at better diagnosing neurological conditions. In October Munsell along with researchers in the departments of psychiatry and radiology at the University of North Carolina Chapel Hill and the School of Software at Tsinghua University in Beijing, China, attended the Medical Image Computing and Computer Assisted Intervention Society’s annual conference in Greece where they presented a new method for analyzing neuroimaging data that assesses impaired brain function.
Creating new techniques to improve the detection of neurological disorders, particularly those afflicting children, is personal for Munsell, who’s 3-year-old daughter Maddy has been diagnosed with a very rare neurological disorder called Alternating Hemiplegia of Childhood.
“Everything I do is for her,” he says.
The new method associated with the IBIS study utilizes refined computational parameters that can detect subtle size increases within specific areas of the brain. These minuscule overgrowth patterns can be indicative of autism.
“It was basically like finding a needle in a haystack,” says Munsell. “To date nobody has really found this with good accuracy before.”
Munsell used the new model to assess the MRI scans of 318 infants with a family history of autism and 117 infants with no family history of autism at six months of age and again at 12 months. Based on increases in brain size, the technique correctly predicted the diagnosis of autism in infants with 94 percent accuracy.

Munsell’s computational approach is able to show significant differences in the surface area of the brain in infants at age 6 and 12 months between typically developing children and children with autism, including the identified regions related to visual processing, word recognition, memory and language processing.
And that’s a big deal, says Munsell, because for the first time it offers doctors a quantitative way to evaluate a child for autism. Previously physicians had no definitive biological way to diagnose the condition. Instead, they have had to rely on a diagnostic test comprised of a series of questions that assessed a child’s behavior at or after the age of two.
With so many significant clinical implications for the new model, the College of Charleston is working with the University of North Carolina to patent the research for further development of the technology.
“This has the potential to help physicians make better decisions for their patients and provide better information sooner to the parents of children at risk for autism,” Munsell says. “That’s why this is so important.”