Gandhi quipped that the best way to find yourself is to lose yourself in the service of others. Like many College alumni doing overseas relief work, Marianne Heis ’06 has discovered the truth behind Gandhi’s statement.
by Marianne Heis ’06
Over the past two years, I’ve seen hundreds of people sleep all night outside a temporary clinic site in Uganda just to make sure they secure a slot with the visiting American medical team the next morning.
I’ve seen a woman wailing on the ground outside the clinic after losing her child to malaria mere hours beforehand. I’ve seen children with third-degree burns all over their bodies from falling into the kitchen fire pit and others with bones sticking out of their arms because they fell three years ago and there was no one around to fix it.
But I’ve also seen healing. Incredible healing. Healing that causes people to jump for joy when they receive a dose of Coartem to treat their child’s malaria or medication to halt their frequent seizures or treat their diabetes. Healing that allows people to see and read for the first time in years, after simply being given a pair of reading glasses. Healing that helps a 10-year-old mute girl speak for the first time, forming sounds and words with her tongue and throat that her family never thought possible, or a 5-year-old walk for the first time after being given supportive braces and therapy. Healing that has allowed more than 11,500 Ugandans to receive quality medical care to date.
If someone had told me I would travel to Africa seven times to help deliver medical care to thousands of people in desperate need, I would have never believed it. I would’ve scoffed: “But I hate hospitals. I don’t know anything about medicine. Of what good could I be?”
Little did I know that an opportunity existed to affect the lives of not only hundreds of compassionate local volunteers from Charleston, but also thousands of people in Uganda who prayed to God to send someone to help them. Someone to love them. Someone to care.
After graduating from the College with a dual degree in communication and political science, I moved to Washington, D.C., to pursue a brief but exciting career in political fundraising. The election cycle ended in November 2008 – and my time in D.C. ended shortly thereafter. I quit my job and joined my church on a mission trip to Choma, Zambia. The experience changed me, and when I returned, I had a burning desire to work for the good of the people of Africa and for the nonprofit community.
The phone rang on New Year’s Day 2009. My good friend Claire Vernon ’06 left a message and said, “I found your dream job, call me!”
Two of her friends in Charleston – Ed O’Bryan and Matt Alexander – were starting a medical nonprofit to focus on sustainable international health care, and they were looking for someone to help with administration and volunteer management for the Palmetto Medical Initiative.
Once word began to spread about PMI’s vision and its dedication to creating a sustainable model, doors began to open. Relationships were extended, opportunities offered and the first project site was determined: Masindi, Uganda.
Masindi is a small town of roughly 30,000 people – about a five-hour drive northwest of Kampala, the capital city. Unfortunately, Uganda’s government system has supplied only the outer shell of a hospital there. Inside, there’s no staff, no medicine and ultimately no care. If you’re admitted, your family or friends are responsible for providing your food, your clothes and the funds for your medicine or prescriptions. There are no meals, very few sanitary standards and definitely no Medicare system. Many people suffer silently. The local community has come to think of hospitals as a place to die, rather than a place to recover. The need for a quality medical system is undeniable.
So when we began sending teams from South Carolina in March 2009 to deliver temporary medical care, the Masindi community responded. Groups of 200–500 Ugandans began to show up at the temporary clinic sites every day for the chance to see a PMI medical volunteer. Many had never seen a doctor before. At one clinic site earlier this year, a translator explained to me that some of the patients had traveled from Sudan to see the medical team.
“Oh, you mean they came from the Sudanese refugee camp down the road?” I asked.
No, he explained, they came from the country of Sudan – traveling more than 11 hours in hopes that they would see someone with medical knowledge. They had heard announcements about the PMI clinic on the radio and knew it was their only hope for help.
Interprofessional PMI teams of both medical and nonmedical volunteers visited Masindi every three months and provided continuous care while a permanent medical center was being built. Teams were and are often comprised of local church volunteers, students and medical personnel from the Medical University of South Carolina – nurses, therapists, doctors, dentists, pharmacists, psychologists and more. Since March 2009, more than 300 volunteers have given up a week of their own time and raised funds for the trip cost.
Over the past two years, plans were finalized for a permanent, sustainable structure in Masindi. We hired a project director from Charleston, Michael O’Neal, who agreed to move to Masindi for two years with his wife to oversee the development of the clinic.
Blueprints were drawn, government permits secured and land cleared. In April 2009, PMI broke ground on the building site and construction officially began on the first phase of the clinic plans – an outpatient building that would serve approximately 500 people every month. Future plans include the construction of three inpatient wards, a surgical ward/labor and delivery center, administration buildings, staff quarters and a physical therapy building. When completed, the clinic will operate at close to 100 percent sustainability, with income being generated by fees charged to patients on a sliding scale.
In December 2010, I was at the opening of the new outpatient building. It was a proud and memorable day for everyone involved. When the December team showed up the next morning to begin working out of the newly constructed building, they were met with hundreds of local people who stood up and began singing praises to God for the team’s arrival. Big bear hugs were exchanged between the local people and the American team, and it was unclear which group felt more blessed by the other’s presence.
Nine local Ugandan medical and administrative professionals have been hired and trained to run the outpatient clinic, and it officially opened for business on January 3. Since then, the Masindi Kitara Medical staff report that they have seen a consistent flow of patients, and many people stop by the site every day simply to say “thank you.”
During our December trip, one of our volunteers reflected on her experience. She was amazed at how the community was responding. She was grateful for the small role she was able to play and said, “When you dream about changing the world, this is how you dream it.”
As I know firsthand, volunteers return with a changed perspective on life and on health care – and many opt to return to Masindi with another team to check up on the progress
and continue investing in that area. Two long-term medical volunteers, Mandie Turner and Rachel Fuller ’05, moved to Masindi to help provide insight and training during the beginning clinic stages.
As we prepare to enter into phase two of the clinic complex construction, we realize that our hardest work lies ahead of us. Many organizations before us have gone into African communities and built medical clinics. The evidence can be seen all around you when driving through the streets of Uganda. Empty buildings with grass growing up in the middle of them are all that’s left from other Good Samaritan organizations with the best of intentions.
The difficult part is ensuring the project’s sustainability and effectiveness. Now the real work begins as we prove our commitment to the area and carry out our vision of quality care, sustainability and partnership with the people of Masindi. The goal is to be able to take this model and replicate it elsewhere – into other needy communities and perhaps other countries.
In my experience, the cliché proves true: The need is great, but the workers are few. But PMI is blessed to be able to link two communities together in a way that will hopefully provide quality, sustainable, long-term change.
– Marianne Heis ’06 is the administrative director at Palmetto Medical Initiative in Charleston and is a graduate student in the College’s M.P.A. program. To learn more about PMI, visit www.palmettomedical.org
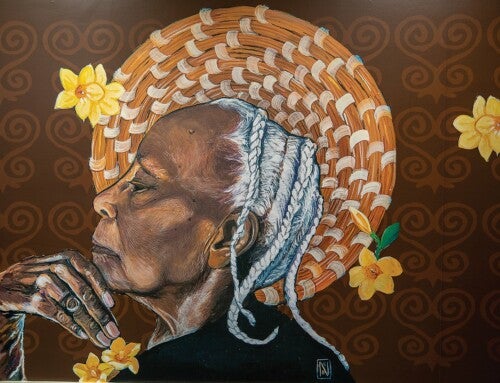
Photo by Joshua Drake